 The case which I will describe now has two fascinating features. Firstly, accurate auscultation led to correct diagnosis, while high technology imaging tests performed previously missed significant lesion. Secondly, the auscultatory picture was very bright, and its careful analysis is edifying.
The case which I will describe now has two fascinating features. Firstly, accurate auscultation led to correct diagnosis, while high technology imaging tests performed previously missed significant lesion. Secondly, the auscultatory picture was very bright, and its careful analysis is edifying.  The case which I will describe now has two fascinating features. Firstly, accurate auscultation led to correct diagnosis, while high technology imaging tests performed previously missed significant lesion. Secondly, the auscultatory picture was very bright, and its careful analysis is edifying.
The case which I will describe now has two fascinating features. Firstly, accurate auscultation led to correct diagnosis, while high technology imaging tests performed previously missed significant lesion. Secondly, the auscultatory picture was very bright, and its careful analysis is edifying. The man in his fifties had Q-wave inferior MI two and half months ago. About one month later this man underwent stenting of LAD and RCA. Now it seems the patient feels good: no angina, no dyspnoea, no signs of heart failure. But this man can walk only about 900 meters. He could not explain why (he was tongue-tied).
I apologise I can not show his ECG here. There was sinus rhythm without any conduction abnormality with pathological Q-waves II, III, aVF and tall R waves in V1-V3 due to the previous MI.
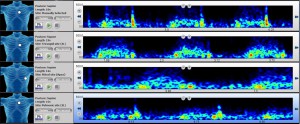
Auscultation was remarkable. Erb’s point, supine position (I strongly advise you listen through headphones):
Here you may hear:
1. Loud pansystolic band-like murmur 3/6. Pansystolic murmur is never innocent, so this murmur is significant. Notice, that murmur does not increase after pauses of premature contractions, so the murmur is not ejection murmur.
2. Widely split S2, near fixed, is abnormal. There are not any conduction abnormality, so the reason of this splitting is haemodynamic.
3. The second component of S2 (pulmonary) is louder than first. Normally pulmonary component is softer.
Tricuspid point:
The murmur is loudest here. Wide splitting of S2 is heard.
Pulmonary point:
The murmur is soft here. Note widely split S2 with accentuated second, pulmonary, component.
Apex of the heart:
The murmur is softer in comparison with tricuspid point. Crucial and rare sign: S2 is still split. It means that we hear aortic and pulmonic components of S2 on the apex. Usually, we can hear only aortic component. So, pulmonary component is abnormally loud.
Let us recap all abnormal findings (Look at the spectrogram above):
1. Loud pansystolic murmur best heard along low and middle sternal border.
2. Widely split S2.
3. Accentuated pulmonary component of S2.
Ok. It seems that pansystolic murmur is the prime sign of the central lesion. What is this lesion? There are only three causes of pansystolic band-like murmur: mitral and tricuspid regurgitation, ventricular septum defect.
The murmur is louder along the left sternal border which is not typical for mitral regurgitation. The loudness of the murmur is nearly constant which is not typical for tricuspid regurgitation (no relation with breath).
Secondly. Loud pulmonary component of S2 heard even over the apex is a sign of pulmonary hypertension.
The pulmonary hypertension is clearly evident. So, we have three possible causes of the murmur:
1 mitral regurgitation
2 tricuspid regurgitation
3 ventricular septum defect (IVS' rupture due to MI?)
It is not difficult to rule out tricuspid regurgitation:
1 the murmur does not depend on breath;
2 jugular veins were normal.
Mitral regurgitation is more frequent than VSD. But the mitral regurgitation’s murmur is louder rather over the apex and cold be transmitted laterally. On the other hand, when the flow of mitral regurgitation is directed anteriorly, the murmur could be well heard over the entire precordial area.
IVS’ rupture leads to VSD and can occur due to MI. Typically its murmur is loudest along the left sternal border like here. But IVS’ rupture is significantly less frequent by comparison with MR.
Wide splitting of S2 could be due to MR and VSD. That is because left ventricle has two outputs in systole: aorta and mitral valve in the case of MR, aorta and VSD in the case of VSD. It decreases LV’s afterload and shortens the ejection time, which leads to earlier closure of aortic valve and earlier occurrence of aortic component of S2, which leads to wide splitting of S2.
So, the wide splitting of S2 can not help us to distinguish confidently between MR and VSD.
The patient was undergone to Echo with one question: VSD or MR?
Watch his Echo:
Here you can see left ventricular regional motion’s abnormality and IVS’ rupture.
Learning points:
The accurate physical examination is vital and power tool.
Key signs of IVS’ rupture:
- Pansystolic band-like murmur along middle and low left sternal border.
- Wide splitting of S2.